Most of us think we know what our doctors are going to tell us: Eat better. Sleep more. Take your vitamins. But the real conversations happening behind closed doors between some doctors and their patients may be more nuanced than that.
They may talk about grip strength as a predictor of independence. They may recommend tracking brain volume for signs of neurodegenerative changes. And they may discuss hidden visceral fat, inflammation, and stress resilience as important markers of future health.
These aren’t influencer wellness trends, it’s the kind of forward-thinking, science-backed advice some doctors may be giving their patients to improve healthspan, not just lifespan.
Here are 8 strategies you might start hearing from your doctor, if you haven’t already.
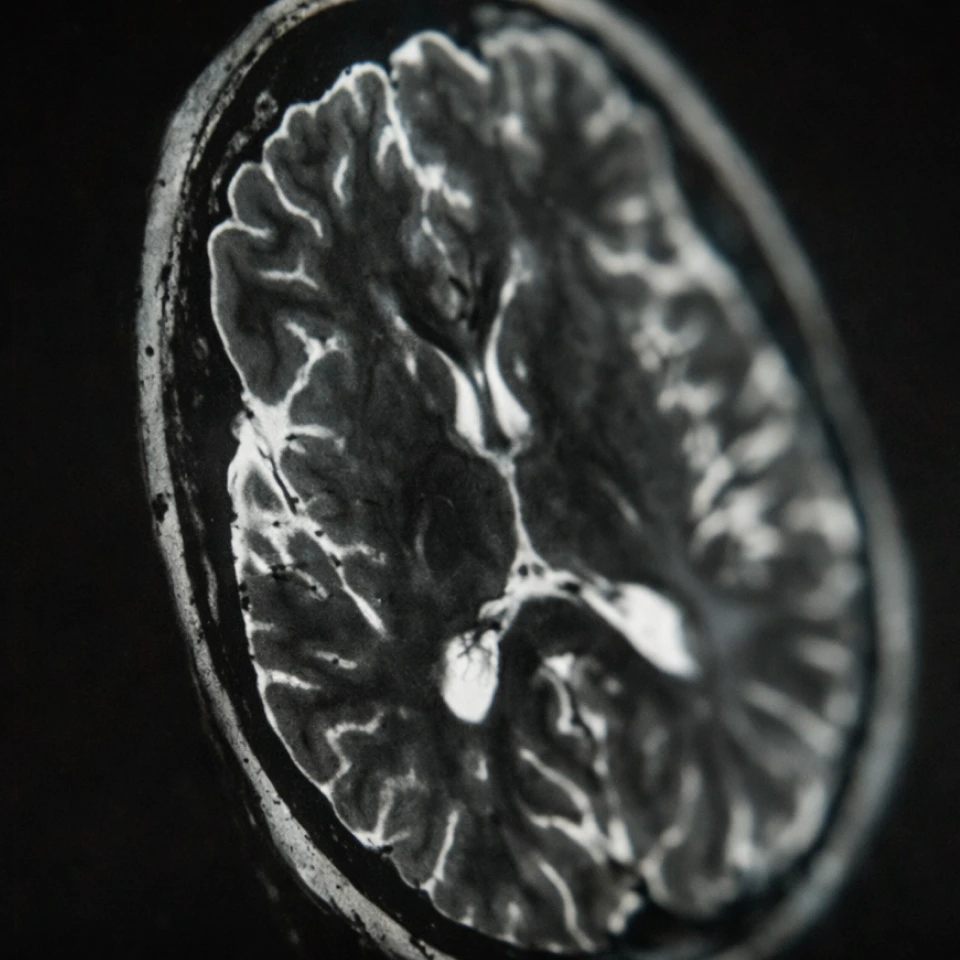
1. Baseline your brain while it’s healthy
Many people may wait until symptoms show up to care about brain health, but some doctors may look at things a bit differently. They understand that structural changes like white matter disease or shrinking brain volume can start decades before memory loss or cognitive issues appear. In fact, recent neuroscientific reviews have shown that the brain naturally undergoes gradual volume loss, changes in gray and white matter, and other subtle degenerative processes with age, even in healthy individuals.
“Tracking brain volume and subtle neurological changes before symptoms appear is a smart thing a healthy adult can do,” says Dr. Shannon Lotus Ashley, M.D., the Senior Preventive Medicine Physician at Prenuvo. “It may help give us a personalized benchmark that helps differentiate normal aging from early signs of neurodegenerative disease,” she adds.
This isn’t about fear—it’s about knowing what “normal” looks like for you, so you can monitor changes long before symptoms may appear.
2. Build your strength, specifically in your grip
“We often think of strength training as a fitness goal, but from a preventive medicine standpoint, grip strength is one of the most predictive markers we have for longevity and independence,” says Dr. Ashley.
It might sound odd, but handgrip strength is a good predictor of long-term health. Studies have linked weak grip strength with increased risk of cardiovascular disease, mobility decline, and even earlier mortality.
That’s why more doctors may tell their patients to lift weights, use resistance bands, and keep their hands strong. Muscle and strength isn’t aesthetics, it’s resilience.
“Both Harvard Health and Mayo Clinic say that two to three days of strength training per week is optimal for muscle, but one day per week is also sufficient,” she adds.
3. Investigate anxiety and/or mood changes
Feeling anxious or low energy? It isn’t always just psychological.
According to Dr. Ashley, symptoms like anxiety and brain fog can also stem from chronic inflammation or metabolic dysfunction, which is why blood markers such as HbA1c, cortisol, and C-reactive protein (CRP) are often checked to understand what’s happening beneath the surface.
Recent research highlights that sustained systemic inflammation and disruption of the blood-brain barrier — a critical defense of brain health — can impair brain signaling and hormone balance, leading to anxiety and brain fog. A 2024 study in Nature Neuroscience linked these inflammatory processes to cognitive symptoms in patients with long COVID, showing a biological connection between inflammation and mental health.
More physicians may begin encouraging their families to track biomarkers like CRP, HbA1c, and cortisol because these tests can provide a clear picture of one’s overall health.
4. Start tracking trends before they shift
One-off lab results can sometimes be misleading. A thyroid level might look “normal” in isolation but still represent a meaningful decline compared to your baseline. That’s why some doctors don’t just check whether your numbers fall within standard ranges, they prefer to monitor how those numbers shift over time.
“Lab results are more powerful when viewed over time,” explains Dr. Ashley. “Subtle shifts in things like cholesterol or thyroid markers can be early signals of change or well before they cross into abnormal territory.”
Take LDL cholesterol, for example. A jump from 90 to 120 mg/dL might still fall within the clinical norm, but for someone with a previously stable profile, it could be a sign of rising cardiovascular risk.
Good preventive care isn’t about reacting to a problem, it’s about spotting a pattern before it turns into one. That starts with establishing a clear baseline while you’re well, then checking in regularly to track the trendlines.
5. Watch for increasing visceral fat
Visceral fat isn’t something you can see in the mirror. It’s the fat that builds up around your organs, deep in the abdomen, and it plays a more serious role in long-term health than many people realize. Unlike body weight or BMI, which can’t distinguish between muscle and fat, visceral fat is strongly linked to metabolic disease, inflammation, and cardiovascular risk. In fact, an internal Prenuvo AI-assisted study of over 7,500 participants found a link between visceral fat and midlife brain atrophy.
That’s why some physicians may often encourage their families to look beyond the scale and focus on internal health.
“Two people can appear equally healthy on the outside, but if one has significantly more visceral fat, their risk profile can be dramatically different,” says Dr. Ashley. “It’s a metric that tells us far more than BMI ever could,” she adds.
Body composition analysis, like in Prenuvo’s Enhanced Screening, allows you to measure visceral fat—giving you a clear picture of what’s happening under the surface.
6. Know your genetic risks early
Your DNA doesn’t determine your destiny, but it can help shape your strategy.
More physicians may increasingly encourage their families to understand their inherited risk factors, not to create anxiety, but to guide smarter decisions. Genetic markers like BRCA1 and BRCA2 (linked to breast and ovarian cancer) and APOE4 (a known Alzheimer’s risk gene) can all influence how a person can screen, supplement, or approach preventive care.
“Genetic insights don’t guarantee outcomes, but they allow us to be proactive—whether that means starting mammograms earlier, supporting brain health more aggressively, or flagging risks that could affect pregnancy,” says Dr. Ashley.
While Prenuvo doesn’t offer genetic testing, it may be worth consulting your doctors about.
7. Build stress resilience like it’s a skill (because it is)
Rather than telling patients to simply “relax more,” more doctors are encouraging the idea of building stress resilience actively with behavioral and physiological tools validated to strengthen the nervous system. Techniques such as cold exposure, breathwork, and HRV tracking train autonomic flexibility. In other words: it teaches the body to recover more quickly and handle stress more efficiently.
“Stress resilience isn’t about eliminating stress,” says Dr. Ashley. "It's about improving recovery and response,” she explains.
A growing body of research shows that regular HRV biofeedback improves emotional control and regulates cortisol response, while repeated cold exposure enhances cellular resilience and mood regulation.
This kind of training doesn’t just make you feel calm, it builds physiological durability. And over time, that can be the difference between burnout and balance.
8. Use whole body imaging and blood labs to establish a true baseline
What are some forward-thinking strategies doctors may recommend? Getting a more comprehensive look at your health, even if you’re not experiencing symptoms.
In just under an hour, a Prenuvo whole body MRI scans for hundreds of conditions and potential abnormalities—from spine health to brain volume and signs of inflammation in the body—providing you with data about your health to use as a baseline that you can measure against in the years to come.
And to go even deeper, a Prenuvo Enhanced Screening can help provide you with even more health information, offering a detailed look at body composition, brain health, and key blood biomarkers tied to metabolism, hormones, inflammation, immune function, and more.
For people who feel healthy, it may offer peace of mind or offer an opportunity to help with early-detection of a treatable condition before symptoms may appear. And for those with concerns that remain unanswered after targeted evaluations, it may offer opportunities for more clarity.
Your health is personal. Treat it that way.
More physicians—and proactive patients—are recognizing the value of acting before illness strikes. Start by establishing your personal baselines for what matters most: metabolic function, brain structure, muscular strength, and systemic inflammation. With your doctor, use those benchmarks to build a plan that supports the future you want.
To learn more about the benefits of whole body MRI and/or Enhanced Screening, book a call with a member of our team.



.jpg)


.webp)
